In the majority of cases, the tests are performed to rule out malignancy or to make an analysis for an increased risk. At the Borstpoli, the intention is always to arrive at a quick, efficient and accurate analysis.
Although a large number of women do not have recognizable breast abnormalities, they may have lumpy, although normal, breast tissue that require further evaluation. Connective tissue nodules or cysts (also known as mastopathy) are the underlying factor in about 40% of all cases. Approximately 10% of women have an abnormality that requires medical follow-up, although in only a few cases is it necessary to go to a hospital for additional testing.
Fortunately, most abnormalities in the breasts of women under the age of 50 are benign; only a few percent are malignant. However, it is important to keep in mind that breast cancer is a relatively common cause of death, especially in women around the age of forty.
In recent years the ultrasound technique has been developed to such an extent that it has become a routine examination, also in hospitals, especially in controlling the breasts of young women. It takes place in order to classify suspicious lumps and to rule out hidden breast cancer, preferably at an early stage. Small lumps that are not seen during a mammography or physical examination are often discovered during an ultrasound. This occurs most frequently in women with firm breasts. It is why ultrasound is the initial research method for girls and young women, who tend to have dense glandular tissue, especially during pregnancy or during breastfeeding. Ultrasound makes it possible for cysts and tumors to be analyzed, while cytology can distinguish various cell types from each other, much like a pap smear.
There’s no question that mammography remains important in the detection of tumors and microcalcifications. Unlike mammography, however, ultrasound is able to detect a tumor as small as 5 mm in any type of breast.
WHAT TO EXPECT
- An intake conversation, during which you’ll be asked the reason for wanting an ultrasound and to describe any physical symptoms you may have.
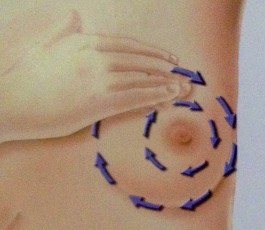
- Physical test in which the doctor inspects the breasts and gives instructions on how to do a self-exam.
- Ultrasound test of the breasts. By using sound waves, the structure of the breast tissue becomes visible. This makes it possible for abnormalities to be detected at an early stage before these can be felt as lumps. This painless method can spot abnormalities less than a centimeter in size, which often means less drastic measures need to be taken.
- Cytological (needle biopsy) test. In the case of abnormalities, the removal of cell material from the breast takes place by means of a fine needle. No anesthetic is used as the puncture is a one-off injection and can be compared to the little jab you feel when your blood is tested. The lump is pricked and the cells that are obtained are spread on a glass slide. This material is then colored and examined microscopically, after which the specialist arrives at an immediate assessment.
SAME DAY DIAGNOSIS
A comparative British study between a specialized breast clinic consultation and a conventional consultation in a hospital where the diagnosis took a week to be conveyed, indicated significantly higher psychological stress linked to the delayed outcome. An immediate diagnosis can substantially reduce uncertainty and stress.
At the Borstpoli, the findings of the ultrasound examination are communicated directly and immediately to the client by the physician. The needle biopsy is also conducted on site and the results of this microscopic examination are conveyed right then and there. The biopsy findings are recorded in writing after being assessed by the pathologist.
INCIDENCE OF BREAST CANCER IN THE NETHERLANDS
Every year, some 9,500 women, 7 percent of whom are below the age of 40, receive a breast cancer diagnosis. This marks the beginning of an emotional rollercoaster and a period of tremendous insecurity for these women. One in 10 women is likely to get breast cancer in her lifetime and more than 3,000 women die each year as the result of this illness.
A breast cancer diagnosis in the family or among one’s friends, as well as coverage in the media, result in many women asking their GP for a mammogram referral, or taking it upon themselves to obtain a mammogram. The demand for breast cancer exams is especially high in the 40 to 50-year-old demographic, which falls outside the official national biannual screenings offered in the Netherlands. There is, however, reason enough to also address the early detection of breast cancer in women who have not yet reached the age of these screenings.
It is important to note that breast cancer is detected in the 40 to 50-year-old demographic nearly as often as in the above-mentioned biannual screenings for women above the age of 50. To date, breast cancer is discovered in the vast majority of cases because the woman feels a lump herself. By the time it’s discovered, this lump generally has a diameter of at least two centimeters. When this is the case, approximately 20 percent of patients already have distant metastases by the time they visit their GP. Smaller tumors can rarely be felt, but these are least likely to have already spread.
Very early discovery, when the nodule is smaller than 1 centimeter and cannot yet be felt, is therefore the ideal early detection for all women, no matter what their age. At the Borstpoli, controls are conducted to ensure an early diagnosis primarily for the group of women under the age of 50 who do not yet participate in the screening program, thus preferably at the moment the lump cannot yet be felt and measures less than 1 centimeter.
A PERSONAL STORY: I Thought a mammogram was enough
I didn’t set out to get an ultrasound. After all, my last mammogram had been just a few months earlier, and it was “clean.” Like all women aged 50-plus who are official residents of the Netherlands, every two years I received a mammogram appointment in the mail. Like clockwork, I’d show up at the “Mammogram Bus”—an oversized trailer supplied with medical equipment and with staff. And I’d always received the all-clear.
But then an old friend—middle aged, like me—was diagnosed with late stage breast cancer. After nearly a decade, several surgeries, and long, grueling periods of chemotherapy, she died. It was her death, at age 58, that prompted me to make an appointment for an ultrasound at the Borstpoli [Breast Clinic] Amstelveen. The clinic had been recommended to me years earlier, by another friend. It couldn’t hurt to have an ultrasound, I reasoned. My friend had told me that ultrasounds give more detailed results than mammograms, and I thought, Why not? Of course the results will be negative. I didn’t have a lump, or any other symptoms. So, by the time of my appointment, I didn’t give it a second thought: I was already thinking ahead to my Pilates class, that afternoon.
The check-up started out routinely enough. Dr. Melkert gave me “the talk” about the importance of checking your breasts correctly (manually examining your left and right breasts at the same time). Then it was time for the ultrasound. Within minutes, I found myself watching the screen as Dr. Melkert indicated a small lesion on my right breast. He considered it suspicious, so he followed up with a Fine Needle Aspiration for Cytology (FNAC).
I still wasn’t worried. Less than half an hour later, though, I received a breast-cancer diagnosis. Just like that.
That same day, I took the Borstpoli results to my family doctor. That same week, I had an appointment with a surgeon, who scheduled me for a mammogram at the hospital. Two days later, the surgeon called me and said my mammogram was negative.
What? Had someone made a mistake? Did I not have breast cancer after all?
No such luck. A subsequent ultrasound and an MRI managed to detect the tumor. So, why didn’t the malignancy show up on the mammogram?
I did some online research, which can be a tricky thing. Sometimes you end up diagnosing yourself—and getting it all wrong. But in this case, I discovered the likely reason the mammogram didn’t detect the tumor. I found a New York Times article—an obituary, sadly—about an American woman, Dr. Nancy Cappello, whose mammograms had also come back clear. By the time an ultrasound diagnosed her breast cancer, the disease had already advanced. When Dr. Cappello asked why mammography had not detected the tumor (Dr. Cappello was not a medical doctor; she was a PhD), her doctors explained the circumstances: she happened to have dense breast tissue, which had hidden the cancer from the X-rays.
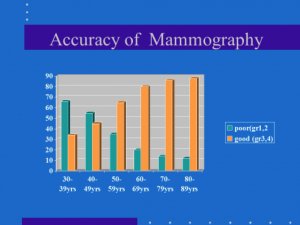
Dr. Cappello had never heard of “dense breast tissue” as a risk factor—and neither had I. Yet up to 50 percent of women who get mammograms have dense breast tissue. Dr. Cappello and her husband made it their mission to get state laws passed to require fuller disclosure to women about dense breast tissue—and the limitations of mammography.
Thanks to the efforts of the Capellos, the majority of states in the US have passed laws requiring women who have mammograms to be informed if they have dense breasts. Recently, the US Food and Drug Administration proposed federal legislation requiring women to receive information about their breast density when they get a mammogram.
In my case, the dense breast tissue—and the tumor it was hiding—were caught in time. Only relatively minor surgery was required to remove the mass. Two weeks after surgery, I had a follow-up appointment with the surgeon to discuss my pathology report. She said she had good news and bad news. The good news was that my lymph nodes were clear: no cancer. The bad news was that my breast cancer was highly aggressive, and I would also need chemo. The surgeon then repeated what I already knew: I was lucky that the cancer was discovered early on. And I knew how that discovery was made—it was the ultrasound.
During the treatment that followed, I couldn’t help thinking about what would have happened if my old friend hadn’t died of breast cancer. What if I hadn’t thought to get the ultrasound? My next mammogram would not have happened until a year-and-a-half later. And who knows whether the malignancy would have been detected even then?
I wonder how many women out there with dense breasts receive mammogram results that appear normal. How many women are reassured—when they shouldn’t be? I wonder whether I would have survived my aggressive breast cancer had I not, impulsively, opted to get an ultrasound in addition to mammograms. Having survived, I feel it’s the least I can do for other women: tell the tale of how I confronted breast cancer, with the help of ultrasound.
COMPLAINTS
Do you have a complaint? Discuss your dissatisfaction with your doctor. If you’re dissatisfied, we would appreciate you discussing this with us. Once we have been made aware of your dissatisfaction, we can try to come up with a solution for you. Borstpoli Netherlands adheres great importance to the quality of its services. If you are dissatisfied or have a suggestion for improvement, please let us know. Submit your comments by sending an email to phc@borstpoli.nl